In recent years, the growing interest in psychoactive substances like MDA and MDMA has led to confusion surrounding their differences, effects, and potential risks. With terms like “Molly” and “Ecstasy” frequently thrown around, it’s essential to distinguish between these substances to better understand their unique chemical properties and their impact on users. In this article, we’ll take a deep dive into what MDA is, how it compares to MDMA, and what users should know about these substances before considering their use.
What is MDA?
MDA, or methylenedioxyamphetamine, is a psychoactive substance that belongs to the amphetamine class of drugs. It is closely related to MDMA, also known as 3,4-methylenedioxymethamphetamine, but it has its own set of effects. MDA is often referred to as the “love drug” because of its euphoric and empathogenic properties. However, it is generally considered more stimulating and slightly less empathetic than MDMA.
The Science Behind MDA
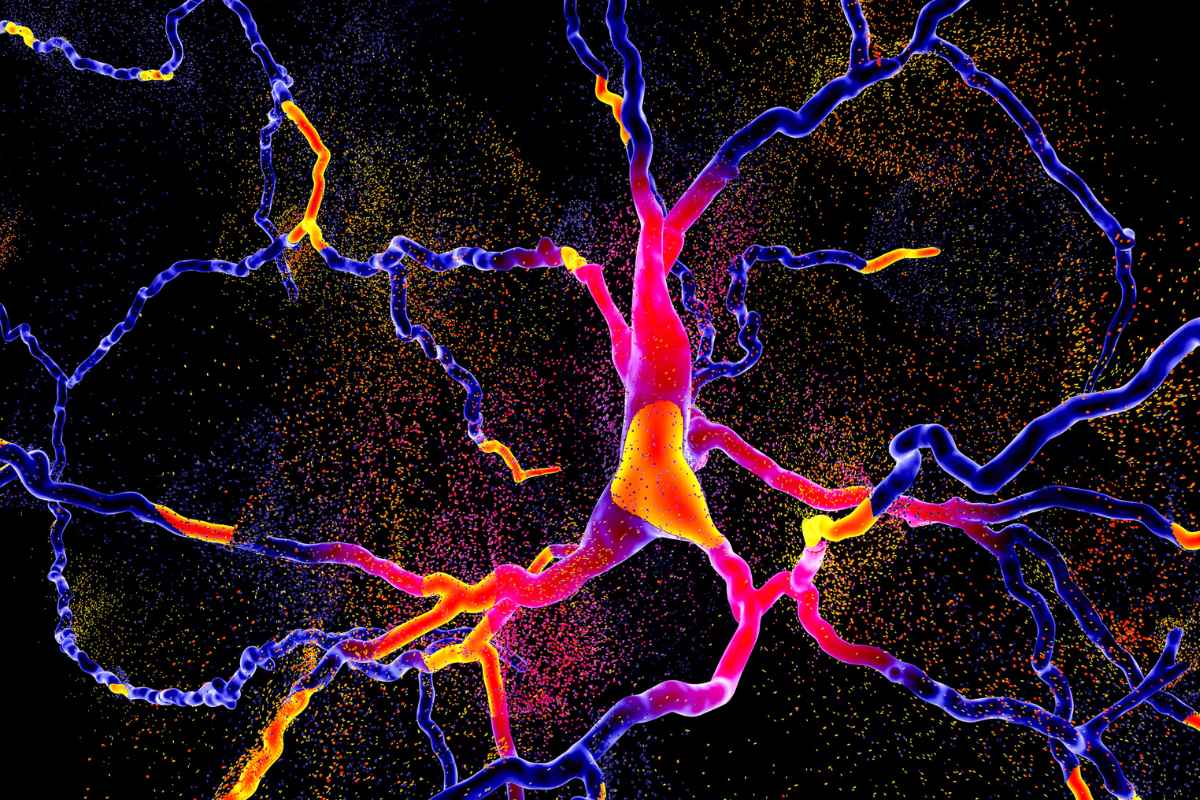
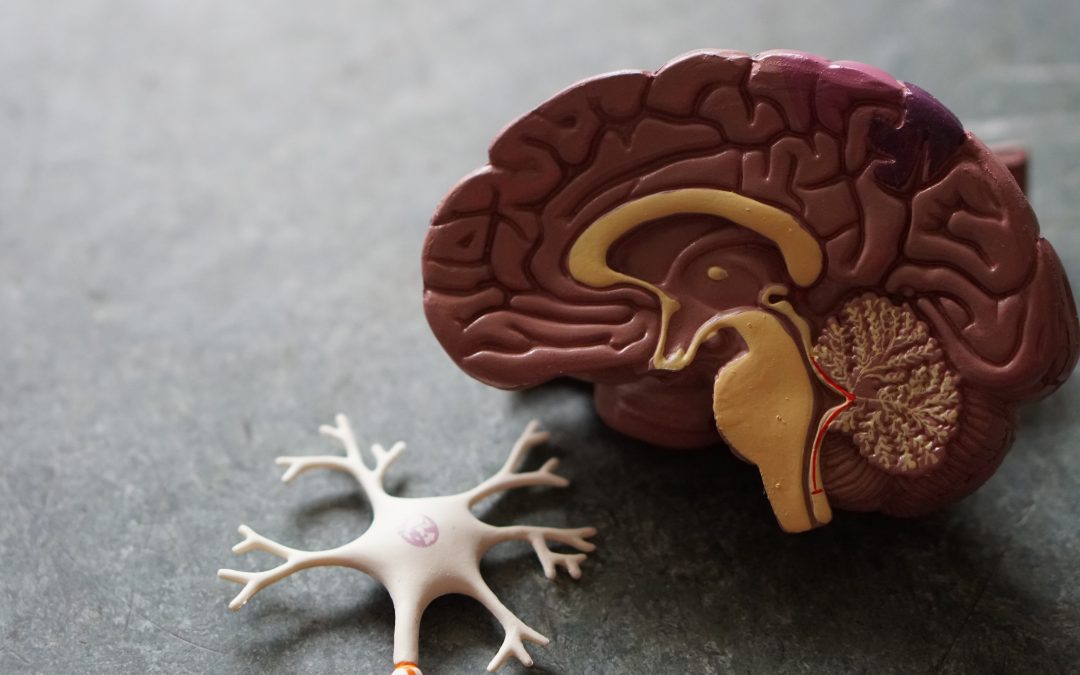
MDA works by increasing the release of serotonin, dopamine, and norepinephrine in the brain. These neurotransmitters are responsible for mood regulation, pleasure, and arousal. The surge in these chemicals can result in feelings of happiness, increased energy, and enhanced sensory perception. While MDA’s effects are similar to MDMA, they tend to last longer, with a more pronounced stimulant effect.
MDA vs. MDMA: What’s the Difference?
One of the most frequently asked questions is: What is the difference between MDA and MDMA? Though they are chemically similar, there are notable differences in their effects and how they are processed by the body.
- Euphoria and Empathy: MDMA is often favored for its intense feelings of empathy, connection, and emotional warmth. MDA, on the other hand, is slightly more stimulating and may not induce the same degree of emotional closeness.
- Duration: MDA typically lasts longer than MDMA. While the effects of MDMA generally last 3-6 hours, MDA can extend up to 8 hours.
- Visual Effects: MDA is known to produce more intense visual hallucinations, whereas MDMA is more about emotional experiences and heightened sensory perception.
- Risk of Overstimulation: Due to its more stimulant nature, MDA may carry a higher risk of overstimulation and anxiety compared to MDMA.
In summary, while both MDA and MDMA share empathogenic and stimulant properties, MDMA is more suited for emotional connection, while MDA offers a more stimulating, psychedelic experience.
MDA vs. Molly: Are They the Same?
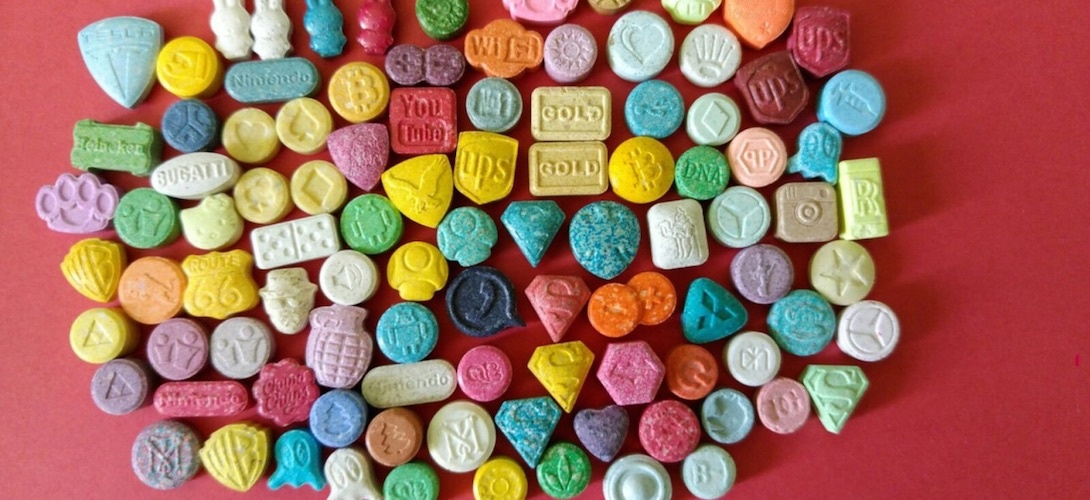
The term “Molly” typically refers to MDMA in its pure form, but it’s important to note that Molly can sometimes be misrepresented. In some cases, what is sold as Molly may contain MDA or other substances. This leads to the question: MDA vs. Molly—what’s the difference?
- Purity: Molly is often marketed as pure MDMA, but it can be adulterated with MDA, methamphetamine, or other chemicals. The risk of unknowingly consuming MDA instead of MDMA is common in unregulated markets.
- Effects: As mentioned, MDA produces more visual and stimulant effects, while Molly (if it is pure MDMA) focuses more on mood enhancement and emotional connectivity.
The overlap in street names and the lack of regulation can make it difficult to know exactly what one is consuming. Testing kits are highly recommended for those considering using these substances.
What is Methylenedioxyamphetamine (MDA)?
To clarify the science, methylenedioxyamphetamine, or MDA, is a chemical compound that belongs to the phenethylamine family. It is similar to MDMA in structure but differs in its effects on the brain. Methylenedioxyamphetamine was first synthesized in 1910 and has since been used in research as well as recreationally.
While MDMA (ecstasy) is often the more popular of the two substances, MDA remains in circulation, often sold under similar names or combined with MDMA. The challenge for users is in distinguishing between the two and understanding how each one may affect them differently.
The Risks of MDA and MDMA
Both MDA and MDMA carry inherent risks, especially when taken in uncontrolled environments. Some of the common dangers associated with these substances include:
Overheating: Both MDA and MDMA increase body temperature, which can lead to dangerous levels of overheating, particularly in crowded environments like concerts or parties.
Dehydration: Users may become dehydrated due to excessive dancing and sweating while under the influence of either drug.
Serotonin Syndrome: Since both substances flood the brain with serotonin, there is a risk of serotonin syndrome, a potentially life-threatening condition that can occur when too much serotonin accumulates in the body.
Psychological Effects: MDA, in particular, can cause heightened anxiety, paranoia, or hallucinations, especially in higher doses.
Unknown Adulterants: As mentioned earlier, one of the biggest risks of using MDA or MDMA is not knowing the true contents of the pill or powder. Substances sold on the street may be mixed with harmful chemicals or even other drugs.
MDA and MDMA in Addiction Treatment
For individuals struggling with the misuse of MDA, MDMA, or similar substances, treatment options are available. Programs like those at All American Detox focus on providing comprehensive care for individuals dealing with substance abuse, including detox and therapy. The recovery process for stimulants like MDA involves a combination of medical support and psychological care.
Understanding the risks associated with MDA use and having access to safe, professional care is crucial for those looking to overcome addiction. All American Detox in Los Angeles offers culturally sensitive and individualized treatment plans to help individuals break free from the grip of drug dependence.
FAQ: MDA and MDMA
1. What is MDA?
MDA, or methylenedioxyamphetamine, is a psychoactive stimulant and empathogen similar to MDMA, but with more intense visual and stimulant effects.
2. How is MDA different from MDMA?
MDA tends to be more stimulating and longer-lasting than MDMA, with stronger visual effects. MDMA, often known for its emotional and empathetic properties, is more focused on emotional connection.
3. Is MDA the same as Molly?
No, Molly typically refers to pure MDMA, but it may sometimes be mixed with MDA or other substances.
4. What is methylenedioxyamphetamine?
Methylenedioxyamphetamine (MDA) is a chemical compound from the amphetamine family known for its stimulant and hallucinogenic properties.
5. What are the risks of taking MDA?
MDA can cause overheating, dehydration, serotonin syndrome, and psychological effects like anxiety and paranoia. There’s also the risk of taking adulterated substances.
6. How long do the effects of MDA last?
The effects of MDA generally last 6-8 hours, longer than MDMA, which typically lasts 3-6 hours.
7. Can MDA lead to addiction?
Yes, MDA can be habit-forming, especially with repeated use. Addiction treatment is available for those struggling with substance abuse.
8. How does MDA affect the brain?
MDA increases the release of serotonin, dopamine, and norepinephrine, causing feelings of euphoria, increased energy, and altered sensory perception.
9. Is MDA illegal?
Yes, MDA is classified as a Schedule I controlled substance in many countries, meaning it is illegal to possess, sell, or use.
10. Can MDA and MDMA be mixed?
Mixing MDA and MDMA can increase the risk of overstimulation and other dangerous side effects.
MDA vs. MDMA – Know the Differences
When considering MDA vs. MDMA, it’s important to recognize their similarities and differences. Both substances have the potential to alter mood, perception, and sensory experiences, but MDA is more stimulating and psychedelic, while MDMA focuses more on emotional connectivity. The risks of using either drug, particularly in unregulated environments, can be significant.
As public awareness of psychoactive substances grows, it’s essential to approach these drugs with caution and seek professional support if misuse occurs. With the help of programs like All American Detox, individuals can navigate the challenges of substance abuse and work towards a healthier, substance-free life.